Vertigo and Dizziness: Causes, Symptoms and Treatment
Free downloadable information packet
Our experts put together a free, comprehensive information packet covering the causes, symptoms and treatment options for vertigo, balance and vestibular disorders. Download the packet here and learn more about vertigo and vestibular disorders in the article below.
What is the Vestibular System and how does it relate to vertigo and dizziness?
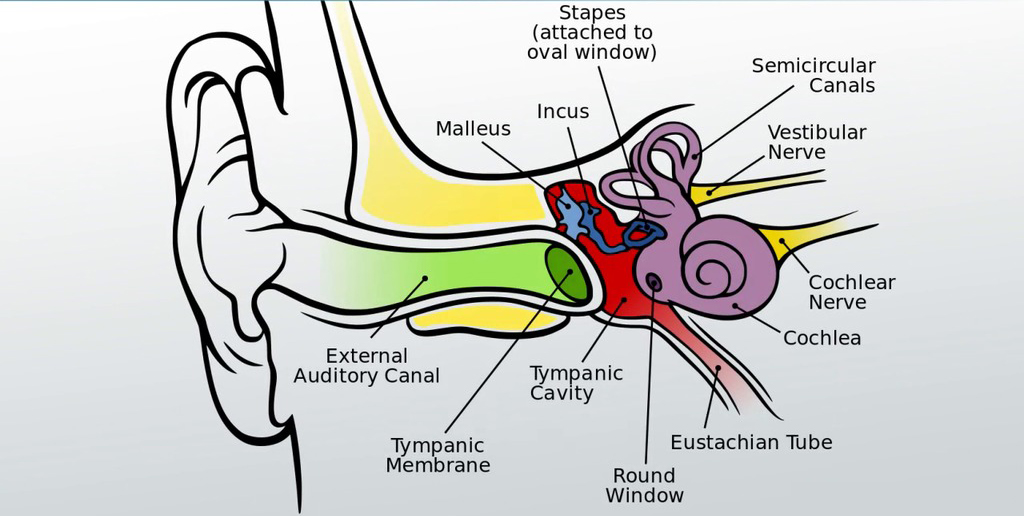
The vestibular system, otherwise known as the human balance system, is critical for our sense of balance, body position, spatial awareness and detecting motion and positioning of the head, such as rotation. It is comprised of a membranous labyrinth of the inner ear, consisting of three semicircular ducts (horizontal, anterior and posterior), two otolith organs (saccule and utricle), and the cochlea.
If disease or injury damages these processing areas, vestibular disorders can result, which can create problems with balance, dizziness and spatial orientation. Vestibular disorders can also result from or be worsened by genetic or environmental conditions, or occur for unknown reasons.
Symptoms of vestibular disorders can include:
- Dizziness and Imbalance
- Sense of Room Spinning
- Spatial Disorientation
- Audio/Visual Problems
- Tinnitus
- Migraine
- Cognitive Changes
 Dizziness and Vertigo: is there a difference?
Dizziness and Vertigo: is there a difference?
People experiencing dizziness often incorrectly say they’re experiencing vertigo, but the two conditions are fundamentally different. While dizziness is often associated with imbalance, light-headedness, and spatial disorientation, vertigo is the sensation that the environment around you is actually moving – that the room is spinning or swaying. Both can be quite distressing and dangerous, but while dizziness can be caused by a number of different issues and disorders, vertigo most commonly has only one cause. See below for details.
Commonly diagnosed vestibular disorders include:
Vertigo – Benign Paroxysmal Positional Vertigo (BPPV): BPPV occurs when tiny calcium crystals (yes, crystals!) in one part of your inner ear are dislodged due to sudden injury or age-related deterioration. This causes your inner ear to tell your brain you’re moving when you’re really not, which means your brain compensates for movement that’s not happening, often causing a sensation of spinning or swaying. Sudden blows to the head that cause concussion can result in BPPV, which is why concussion is sometimes associated with short or long-term vertigo.
Labyrinthitis and Vestibular Neuritis: Often occurring due to an ear infection or viral infection, Labyrinthitis and Vestibular Neuritis can cause balance problems, dizziness, nausea and vomiting, as well as ear pain and headaches.
Ménière’s disease: Caused by too much fluid in the ears due to allergies or infection, Ménière’s disease can present as tinnitus, hearing loss and a feeling of “fullness” in the ear (kind of like getting water in your ear while swimming). It can be painful, disorienting, and can eventually cause permanent hearing loss.
Vestibular migraines: Vestibular migraines or associated headaches can occur if your brain sends the wrong signals to your balance system. Other symptoms can include dizziness, sensitivity to light or sound, hearing loss, tinnitus and blurred vision.
Autoimmune Inner Ear Disease: An inflammatory condition, Autoimmune Inner Ear Disease (AIED) is caused by an uncontrolled immune system response that attacks the inner ear. It can cause progressive hearing loss that usually starts in one ear and then affects the other ear, as well as tinnitus, dizziness and balance problems.
How can physical therapy help?
Vestibular Rehabilitation Therapy (VRT) is a form of physical therapy that is intended to alleviate issues caused by vestibular disorders. Programs are exercise-based and designed to reduce symptoms.
The goal of VRT is to identify each individual’s problem(s) and then create a custom program of guided movements and exercises to promote “compensation,” or actions that can compensate for the disorder to correct them. Before this program can be designed, a comprehensive clinical examination is done to pinpoint the issues related to the vestibular disorder and offer a diagnosis.

Depending on the vestibular-related disorder(s) identified, three primary methods of exercise can be prescribed. These methods, comprised of guided movements, exercises and practices, address the specific disorder(s) of each patient with the goal of alleviating immediate symptoms, decreasing the intensity and frequency of recurring symptoms, and teaching the patients ways to mitigate them on their own. They include:
1) Habituation: aimed at treating dizziness and other symptoms by identifying certain movements that may be bringing on the symptoms, and then performing the movements in controlled sessions in order to “normalize” the brain’s response to them.
2) Gaze Stabilization: aimed at addressing symptoms that include bouncing or shaking vision, the patient is guided through exercises to improve control of eye movements so vision can be clear during head movement.

3) Balance Training: focused on identifying weaknesses and balance issues, and then performing guided exercises to strengthen and improve balance, while also assessing environmental fall risks.
*For BPPV (Vertigo), sessions may also include movements, exercises and best-practices for mitigating the “spinning-sensation” often associated with the disorder.
Vestibular Rehab Therapy often covers:
- Visual and/or somatosensory cues
- Stationary positions and dynamic movements
- Coordinated movement strategies (movements from ankles, hips, or a combination of both)
- Dual tasks (performing a task while balancing)
- Ability to walk on uneven ground or in the dark
- Balance while standing, bending, reaching, turning and walking
If you’re experiencing a suspected vestibular issue, or if you have dizziness, headaches or balance issues, request an evaluation at your nearest PTSMC clinic and get an expert assessment. See a full list of our locations here.
Learn even more in this comprehensive presentation by Jen Ashman of PTSMC Simsbury below!